Medical care delivery is under tremendous pressure to to improve productivity. This is not surprising since health care delivery has taken an almost century long hiatus from productivity growth. However, the pressures and incentives now being applied may have unintended and not productivity- enhancing consequences. They may drive volume growth but not necessarily value growth.
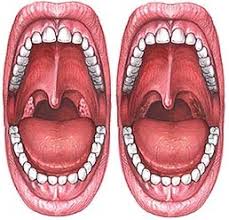
I am reading the iBook version of "Tracking Medicine" by John Wennberg. This work describes the work which served as the basis for the Dartmouth Atlas. His description of the variation of tonsillectomy rates in adjacent communities is really priceless. He focuses on the heuristics utilized by three different surgeons to justify the use of tonsillectomy. One stresses anterior tonsillar pillar injection while a second dismisses this finding and instead focuses on adenopathy. A third dismisses both of these. As one other, perhaps more reflective surgeon noted, the only reason to look at the throat is to make sure that someone had not gotten there first and there are still tonsils to remove.
The point is there is much belief and little actual data and that each physician had developed a quick approach with a bias toward action. Those surgeons whose approach required them to be more thoughtful and reflective ended up being less productive in the sense they took longer to decide to do nothing, or at least what appeared to be nothing.

I could go on and on with examples where the medical profession has evolved toward the use of heuristics which are unsupported by outcomes data where their use is driven by the ability to deploy them quickly and link them to the use of some revenue generating activity. Rapidly these activities become embedded within practice, becoming both lucrative and defining standard of care. Under these circumstances who in their right mind is going to go out on a limb and refuse to do something which both pays their bills and is expected by patients and colleagues alike, even if it adds nothing of value to patients?
The way out of these quandries is actual outcomes data and changes in payments which reward real gains in productivity which includes value measures, not just volume measures. How this will end up looking is anyone's guess.
No comments:
Post a Comment