I had a very interesting conversation with colleagues tonight regarding optimizing communications within a health care network. It has always been a pet peeve of mine that communication networks among physicians tend to be very ad hoc in their functioning and information exchange. There was agreement within the group that something needed to be done. However, there was no consensus on exactly what optimal communication strategies should look like.
One of my colleagues who is an orthopedic surgeon, thought the best tool for his communication needs was the phone. It was his opinion that this approach afforded him with the fastest way to get the information he needed to ascertain whether he needed to see the patient or not and he was perfectly willing to use his time in a non-compensated fashion to avoid filling one of his new patient slots with a patient that would not feed his operative machine. For him, it seemed that the only reason to communicate with his fellow docs was to make sure that he did not interrupt the flow of good operative candidates into his office. There were merits in this communication approach in that it can address the concerns of primary care physicians and patients in real time and perhaps serves their immediate needs.
Still I have somewhat of a different perspective on the need for synchronous, real time communication, particularly by using the phone. When that encounter he describes is over, the only record of what was asked and what was said exists in various parties' minds. Presumably there was some sort of information shared with the consultant, some of which he heard, some of which he did not, and of the part he heard, there is some fraction of that he retained. In response, he made an assessment which was communicated to the consulting party, likely with a set a recommendations. What parts of the assessment and recommendations were heard and retained by the consulting physician shares the same limitations.
At some point, the assessment and recommendations get transmitted to some part of the medical record. I would venture to guess that at least part of this will be attributed to the physicians who gave his recommendations over the phone. How closely these track with what was said or intended is anyone's guess. Whether this note gets forwarded to the consultant is unlikely, meaning in some sense hearsay is documented in the medical record. Alternatively, nothing is recorded at all. It may be that none of this actually matters in that little or nothing was really at stake. Who really knows? We will never know since the record of this type of encounter and call will always be incomplete and error filled until we deploy software which records and parses everything we say and hear.
Am I being a nit picker about this? Is accurate communication important when dealing with someone's health? Imagine the legal system where a similar standard for communication was used? What is it about health care where we settle for spoken instructions and written records riddled with errors and imprecision?
I think this is part of a much larger issue regarding the best use of information to support decision making and coordination of care. Neither of these tasks are really priorities in the current world. Information collection is ad hoc. Decision making is very intuitive and system one based. In a world where there are few consistent feedback loops, any decision which is roughly equivalent in terms of financial outcomes becomes acceptable. Coordination of care is much talked about but also done in an ad hoc manner with no real rules of engagement. I talk to you and you talk to me. I think I hear what you tell me and you think that you hear what I tell you. I think I get what I want and you think you get what you want, and no one has any real idea of whether the patient gets what they need, unless their only priorities are to be dealt with quickly but not necessarily effectively. We prioritize speed and "efficiency" and that is what we get, nothing more and nothing less.
Definitely not a follower: Following the herd will get you to where the herd is going
Saturday, June 28, 2014
Thursday, June 26, 2014
Unbridled Power - The IRS and record keeping
The latest news regarding the IRS and emails reminded me of a book I read over 15 years ago titled "Unbridled Power: inside the secret culture of the IRS" by Shelley Davis. Ms. Davis was the first and likely last official historian of the IRS. She had a long career as a government historian, working for the Air Force and Defense Department Mapping agency before her employment at the IRS.
Throughout the federal government, there a professionals whose job is to manage documents in their agencies, reviewing them and forwarding relevant ones to the National Archives. This is what Mrs. Davis did in her previous roles in the Department of Defense. When she arrived at the IRS she discovered that the IRS basically had no clear record retention policy and were engaged in a struggle with the National Archives to resist archiving IRS records. She testified to this effect to before the Senate finance Committee Oversight Hearing on Internal Revenue Service, Tuesday, September 23, 1997 (Shelley Davis Senate Testimony).
From her testimony:
 Does this sound familiar? While at first I simply could not believe that the IRS could believe they could get away with such flagrant abuse of the law, I now realize that why shouldn't they believe so. They have been doing this for years. Shred paper documents or shred hard drives. What is the difference?
Does this sound familiar? While at first I simply could not believe that the IRS could believe they could get away with such flagrant abuse of the law, I now realize that why shouldn't they believe so. They have been doing this for years. Shred paper documents or shred hard drives. What is the difference?
This has been going on for years. 1997 GAO report
Throughout the federal government, there a professionals whose job is to manage documents in their agencies, reviewing them and forwarding relevant ones to the National Archives. This is what Mrs. Davis did in her previous roles in the Department of Defense. When she arrived at the IRS she discovered that the IRS basically had no clear record retention policy and were engaged in a struggle with the National Archives to resist archiving IRS records. She testified to this effect to before the Senate finance Committee Oversight Hearing on Internal Revenue Service, Tuesday, September 23, 1997 (Shelley Davis Senate Testimony).
From her testimony:
My introduction to the culture of the IRS came during my earliest days with the tax agency, in the fall of 1988. Although I had been hired as the first historian for the IRS, I found little interest or support for my efforts. I found even less history. By history I mean both an awareness of the heritage of the IRS as well as the raw material (the documentation) from which narrative history is distilled. Neither the documents nor the heritage were to be found. Initially, I found this curious. Later, I found it alarming. At the IRS National Headquarters, there seemed little connection between the work of employees and actual tax collection what I presumed to be the mission of the IRS. Rather than possessing any basic curiosity about the past, the IRS employees I encountered exhibited a wariness, a suspicion assuming that anyone looking for records must have some definite agenda. An agenda presumed to be negative.
This reluctance to think about the past translated into routine day-to-day operations, meaning that all documents were tossed, shredded, whatever, when a program was completed or shut down, as in the case of many IRS computer projects. No records. No paper trail. No history.......
......A corollary to this defensive shield is the penchant of the IRS to destroy its paper trail. There were virtually no records of IRS actions throughout the twentieth century in any of the repositories where one would normally find federal records: the IRS itself, the National Archives (including the permanent archives in Washington, D.C., the 10 records centers around the country, or the Presidential libraries.)
In my early years with the IRS, a good question to ask was, "Where are the records?" What I learned was shocking. The records had been destroyed. Gone. Shredded. Tossed. They no longer exist due to a lack of attention to, or concern for, the law which requires all federal agencies to preserve records of what they do. It is as though the IRS assumed that laws which apply to the FBI, to the CIA, to every other part of the federal establishment can be ignored. No other agency of our government could get away with this. I questioned the reason why it had taken so long for anyone to realize that the records were not just missing, but destroyed. I believe the answer is based on fear. As taxpayers, why would we ever question the one agency that can truly bite back?
This has been going on for years. 1997 GAO report
Monday, June 23, 2014
Worth watching
All about what people want as opposed to what they need
and a contrary perspective:
http://reason.com/blog/2014/06/28/baylen-linnekin-defends-dr-oz-and-free-s?utm_source=feedburner&utm_medium=feed&utm_campaign=Feed%3A+reason%2FHitandRun+%28Reason+Online+-+Hit+%26+Run+Blog%29
and a contrary perspective:
http://reason.com/blog/2014/06/28/baylen-linnekin-defends-dr-oz-and-free-s?utm_source=feedburner&utm_medium=feed&utm_campaign=Feed%3A+reason%2FHitandRun+%28Reason+Online+-+Hit+%26+Run+Blog%29
Saturday, June 14, 2014
Telling people "You should not want that"
We are increasingly steeped in the evidenced based medicine culture. In a nutshell, this culture promotes interventions which we can demonstrate objectively that patients benefit from. Interventions which fail to demonstrate positive benefits are viewed with skepticism. I am very much a data driven person and I embrace the idea that if I am to push something as adding value to patients lives, I want to have a substantial degree of confidence that it really does accomplish this.
However, throughout the health care delivery system we are grappling with a very difficult problem. Patients frequently desire interventions which evidenced based enthusiasts believe provide them little or no value. We find ourselves taking time to convince patients that "You should not want this".
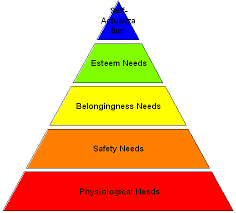
Our measurements and assessments are based upon the rational patient and doctor model. Measuring what we measure to assess value, we conclude that no rational person presented this evidence should want to have particular interventions or tests done. However, human needs are not always based upon rational desires and the value provided by a host of medical interventions and tests may not be what we think them to be. The actual value which patient derive may be based upon fears and wants which are emotionally based and have little or no basis in what we view as solid evidence of benefit.
As an example I can point out the entire industry based upon screening for early disease. Companies send mobile vans with testing equipment into a host of environments. The idea is there is the potential to reach patients who might benefit but because of accessibility issues, are not normally reached. However, those reached also who are already undergoing care who seek out these additional interventions because they provide some additional level of reassurance which they derive from the believe this action provides some additional protection from bad outcomes. Patients under the care of dermatologists go to skin cancer screenings, patients under the care of their internists get free PSA or lipid panels at the mall, and patients under the care of cardiologists pay additional sums to get a scan to look for calcium in their cardiac vessels from the van cruising their streets.
 Another example is the recent decision of Medicare to cover gender reassignment surgery. This is the quintessential example of where human needs and wants are confused and confusing. There is absolutely no objective measure which can be used to justify this specific human desire, to change one's sex. If it is acceptable to say that there is a medical indication for this particular intervention based upon this unique set of human desires, I am hard pressed to find any other human emotional desire which cannot be justified similarly. Whether one medical professional or another believes it unwise for a particular patient to desire a particular intervention based upon some sort of objective criteria becomes completely irrelevant, no matter what the data might show.
Another example is the recent decision of Medicare to cover gender reassignment surgery. This is the quintessential example of where human needs and wants are confused and confusing. There is absolutely no objective measure which can be used to justify this specific human desire, to change one's sex. If it is acceptable to say that there is a medical indication for this particular intervention based upon this unique set of human desires, I am hard pressed to find any other human emotional desire which cannot be justified similarly. Whether one medical professional or another believes it unwise for a particular patient to desire a particular intervention based upon some sort of objective criteria becomes completely irrelevant, no matter what the data might show.
Based upon everything we know, patients should not want particular things but some (many?) do, because at an emotional level, these actions provide something which makes them feel better. This type of behavior is not unique to customers buying products in the health care arena. We purchase many products where either the product provides little or no objective benefit or we move to a higher end of the market to purchase higher priced variants which provide no greater objective value than the more basic products that can be obtained at steeply lowered costs.
We humans have desires which cannot be explained by the objective outcomes which can be measured. That we believe that the mechanisms to meet health care needs and wants can be segmented from the mechanisms we use to meet rest of human wants and needs is simply folly. We end up telling people that they shouldn't want things that they want, not really understanding their motivations and denying human nature.
However, throughout the health care delivery system we are grappling with a very difficult problem. Patients frequently desire interventions which evidenced based enthusiasts believe provide them little or no value. We find ourselves taking time to convince patients that "You should not want this".
Our measurements and assessments are based upon the rational patient and doctor model. Measuring what we measure to assess value, we conclude that no rational person presented this evidence should want to have particular interventions or tests done. However, human needs are not always based upon rational desires and the value provided by a host of medical interventions and tests may not be what we think them to be. The actual value which patient derive may be based upon fears and wants which are emotionally based and have little or no basis in what we view as solid evidence of benefit.
As an example I can point out the entire industry based upon screening for early disease. Companies send mobile vans with testing equipment into a host of environments. The idea is there is the potential to reach patients who might benefit but because of accessibility issues, are not normally reached. However, those reached also who are already undergoing care who seek out these additional interventions because they provide some additional level of reassurance which they derive from the believe this action provides some additional protection from bad outcomes. Patients under the care of dermatologists go to skin cancer screenings, patients under the care of their internists get free PSA or lipid panels at the mall, and patients under the care of cardiologists pay additional sums to get a scan to look for calcium in their cardiac vessels from the van cruising their streets.
Based upon everything we know, patients should not want particular things but some (many?) do, because at an emotional level, these actions provide something which makes them feel better. This type of behavior is not unique to customers buying products in the health care arena. We purchase many products where either the product provides little or no objective benefit or we move to a higher end of the market to purchase higher priced variants which provide no greater objective value than the more basic products that can be obtained at steeply lowered costs.
We humans have desires which cannot be explained by the objective outcomes which can be measured. That we believe that the mechanisms to meet health care needs and wants can be segmented from the mechanisms we use to meet rest of human wants and needs is simply folly. We end up telling people that they shouldn't want things that they want, not really understanding their motivations and denying human nature.
Thursday, June 12, 2014
Telehealth and the absurdity of "place"
I have become very active in the delivery of health care via remote tools. This is one arena where the VA system is leapfrogging the civilian health care sector. The VA does not worry whether a telehealth encounter is billable. If it deliver the service faster at lower cost, so be it.
Our attempts to apply similar principles outside of the VA have been more challenging and shed light on a legacy model of care which is fixated on a host of details where are essentially divorced from actually adding value to patients. In order to fully appreciate just how off target these concerns are, it is helpful to simply step back and ask the questions:
1. What do we as physicians (and other health care workers) actually do which enhances our patient's lives?
2. What information do we need in order to succeed in these specific endeavors?
3. When communicating with patients and assisting them in making decisions, what approaches are optimal?
4. What role do direct, face to face encounters have in facilitating these activities which are central to delivery of services and adding value to our patients?
The last question is really the key one since the current payment system hold on to an uncompromising link between payment to the practitioner and some sort of real time and direct link to the patient. No face to face real time encounter, no payment. It prompts me to ask the obvious question, why? Is there overwhelming data that demonstrates that such an encounter is essential to the collection and processing of information critical for the diagnostic encounter or to the communication and shared decision making in a time frame most conducive to optimal care. I think not.
From my perspective, the hurried nature of the current models is awful. We force people to wait in "waiting rooms", waiting for their paltry 15 minutes of doctor time. The incentives are to try to do everything you can because any work done outside the confines of this frantic quarter of an hour does not count for billable work. Furthermore, it is all driven my how we are paid.
Current approved (billable) methods of telehealth drive to recapitulate the dysfunctional office encounters in the virtual world. We must stop thinking about telehealth in the terms and instead think about what we want to accomplish, what information do we need, how best to communicate, and which of those functions outlined above can be done remotely. The answer is basically all of them and they can be done better, as long as we stop trying to reconstitute the current model at a distance.
 This perspective creates a whole new series of challenges relating to licensure. At this point in time, I still practice office based medicine. Patients come to me, where I practice in a state where I hold a license. However, some of these patients come from neighboring states. In addition, there are times where I may call them in follow up or communicate with them in some way. I may use a secure patient portal or my cell phone. I have no idea where they might be at the time and after they answer, I still have no idea where they are. I might be out of state when I answer and they might out of state or out of the country.
This perspective creates a whole new series of challenges relating to licensure. At this point in time, I still practice office based medicine. Patients come to me, where I practice in a state where I hold a license. However, some of these patients come from neighboring states. In addition, there are times where I may call them in follow up or communicate with them in some way. I may use a secure patient portal or my cell phone. I have no idea where they might be at the time and after they answer, I still have no idea where they are. I might be out of state when I answer and they might out of state or out of the country.
Does that mean I am in violation of state licensing laws, if I make diagnostic or therapeutic decisions and I happen not be be in the state where I am licensed at the time I am making these decisions? Similarly, if the patient who I am caring for is in another state when they are reading my instructions, is that a violation? Should they be required to come back into the state where I am licensed to read my instructions?
As the exchange of information and the delivery of care becomes less visit based and moves to a more continuous and remote data collection model, what is the meaning of the term "place" when discussing where care is delivered? Will we be required to put GPS devices on both our patients and ourselves and refuse to render care if either patient or provider is outside the licensed domain? Unless we freeze the current dysfunctional model in place, we are going to have to rethink state based licenses and the idea that care is delivered in one place.
Our attempts to apply similar principles outside of the VA have been more challenging and shed light on a legacy model of care which is fixated on a host of details where are essentially divorced from actually adding value to patients. In order to fully appreciate just how off target these concerns are, it is helpful to simply step back and ask the questions:
1. What do we as physicians (and other health care workers) actually do which enhances our patient's lives?
2. What information do we need in order to succeed in these specific endeavors?
3. When communicating with patients and assisting them in making decisions, what approaches are optimal?
4. What role do direct, face to face encounters have in facilitating these activities which are central to delivery of services and adding value to our patients?
The last question is really the key one since the current payment system hold on to an uncompromising link between payment to the practitioner and some sort of real time and direct link to the patient. No face to face real time encounter, no payment. It prompts me to ask the obvious question, why? Is there overwhelming data that demonstrates that such an encounter is essential to the collection and processing of information critical for the diagnostic encounter or to the communication and shared decision making in a time frame most conducive to optimal care. I think not.
From my perspective, the hurried nature of the current models is awful. We force people to wait in "waiting rooms", waiting for their paltry 15 minutes of doctor time. The incentives are to try to do everything you can because any work done outside the confines of this frantic quarter of an hour does not count for billable work. Furthermore, it is all driven my how we are paid.
Current approved (billable) methods of telehealth drive to recapitulate the dysfunctional office encounters in the virtual world. We must stop thinking about telehealth in the terms and instead think about what we want to accomplish, what information do we need, how best to communicate, and which of those functions outlined above can be done remotely. The answer is basically all of them and they can be done better, as long as we stop trying to reconstitute the current model at a distance.
Does that mean I am in violation of state licensing laws, if I make diagnostic or therapeutic decisions and I happen not be be in the state where I am licensed at the time I am making these decisions? Similarly, if the patient who I am caring for is in another state when they are reading my instructions, is that a violation? Should they be required to come back into the state where I am licensed to read my instructions?
As the exchange of information and the delivery of care becomes less visit based and moves to a more continuous and remote data collection model, what is the meaning of the term "place" when discussing where care is delivered? Will we be required to put GPS devices on both our patients and ourselves and refuse to render care if either patient or provider is outside the licensed domain? Unless we freeze the current dysfunctional model in place, we are going to have to rethink state based licenses and the idea that care is delivered in one place.
Subscribe to:
Comments (Atom)